Simulation technologies for optimising COVID-19 drug therapies
June 30, 2022NUS pharmaceutical scientists have developed a modelling and simulation strategy to evaluate the pharmacotherapy of COVID-19 related drugs and help guide dose adjustments for those in the vulnerable population.
There is great public interest regarding the drugs that were granted Emergency Use Authorizations (EUAs) by the United States Food and Drug Administration (FDA) for the treatment of COVID-19. These drugs include both Paxlovid and baricitinib. Paxlovid received its EUA in December 2021 for the treatment of non-hospitalised patients with mild to moderate COVID-19 at risk of progression to severe infection. Baricitinib, a medication typically used for the treatment of rheumatoid arthritis, was also issued with an EUA in November 2020 for the treatment of COVID-19 in hospitalised patients requiring supplemental oxygen. Both drugs are also prescribed for COVID-19 patients in Singapore.
The lack of full FDA approval during the public health emergency would mean that dosing information for these two drugs may be lacking for the adults in older age groups. Also, clinical trials could not be performed in a timely manner for this vulnerable cohort during this period. Multiple chronic health conditions and polypharmacy often accompany older adults and it is expected to take many years to complete the complex risk evaluation involved. This sets barriers for clinicians to make suitable decisions on an optimal COVID-19 drug therapy for their older patients.
To address this clinical conundrum, Professor Eric CHAN from the Department of Pharmacy, National University of Singapore, developed a modelling and simulation strategy to evaluate the pharmacotherapy of two COVID-19 drugs, Paxlovid and baricitinib, under various virtual clinical scenarios. The research team utilised an approach termed as physiologically-based pharmacokinetic (PBPK) modelling to simulate the pharmacokinetics of their target drugs among virtual populations. This methodology has been accepted by FDA in several drug labels for dose recommendations in recent years as an alternative to real-world studies.
For Paxlovid therapy, the research team identified potential risks of drug-drug interactions for a specific group of patients through the PBPK-based simulation. These are COVID-19 patients with cardiovascular diseases and already undergoing treatment using anticoagulants, either rivaroxaban or warfarin. From their simulation outcomes, the team found a significant increase in bleeding tendency when the older patients are on rivaroxaban. Those receiving warfarin treatment are found to suffer from an increased risk of potential thrombotic events.
Dr Ziteng WANG, one of the team members said, “We suggest dose adjustment of rivaroxaban to mitigate the risk of internal bleeding and up to two-weeks surveillance for warfarin treatment after Paxlovid discontinuation to avoid warfarin-related thrombosis.”
In a separate study, the team analysed the current dosage strategies of baricitinib, which was evaluated to be broadly adequate for older adults, except for those with mild renal dysfunction, who might benefit from a dose reduction by half.
Prof Chan said: “Our results provide scientific evidence for the rational dose adjustments of COVID-19 drugs and co-medications in a vulnerable cohort, who are underrepresented in current clinical guidelines. These novel findings are pertinent in supporting further clinical studies and systematic analyses of real-world data to ensure efficacious and safe COVID-19 drug therapies.”
Dr Tat Ming NG, principal pharmacist (specialist) at the Tan Tock Seng Hospital, Singapore, commented, “PBPK modelling is a mechanistic and quantitative approach in understanding how the human body absorbs, distributes, metabolises and excretes drugs under different scenarios that are influenced by intrinsic (age, disease, ethnicity, gender, genetic, pregnancy) and extrinsic (drug, food, smoking) factors. In terms of the treatment for COVID-19, the findings will be useful to help guide clinical scenarios where these drug interactions cannot be avoided.”
The team plans to extend their virtual simulation strategy in the evaluation of other COVID-19 drugs to clinically relevant yet untested clinical scenarios.
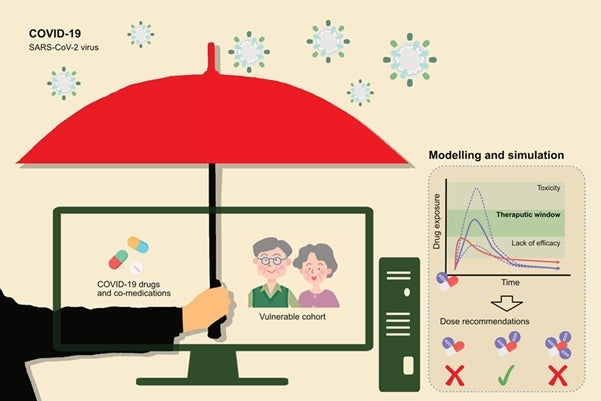
Visual giving an impression of how the modelling and simulation strategy could help optimise drug therapies and protect vulnerable patients from COVID-19.
References
Wang Z; Chan ECY*, “Physiologically Based Pharmacokinetic Modelling to Investigate Baricitinib and Tofacitinib Dosing Recommendations for COVID-19 in Geriatrics” CLINICAL PHARMACOLOGY & THERAPEUTICS DOI: 10.1002/cpt.2600 In Press.
Wang Z; Chan ECY*, “Physiologically Based Pharmacokinetic Modelling-Guided Dose Management of Oral Anticoagulants when Initiating Paxlovid for COVID-19 Treatment” CLINICAL PHARMACOLOGY & THERAPEUTICS DOI: 10.1002/cpt.2687 In Press.


