Non-sex hormones in sexing liver cancers
August 07, 20177 Aug 2017. NUS biologists have discovered that two hormone factors, cortisol and serotonin, play critical roles in the development of male-biased liver cancers.
Liver cancer is a sex-biased disease. It occurs more frequently in males than females. This gives an impression that sex hormones might be involved in the development of liver cancers. However, clinical trials targeting sex hormones did not produce sufficiently convincing results, suggesting that other factors might also be involved. Liver cancer models based on zebrafish also show sex disparity. In particular, two non-sex hormone factors, cortisol and serotonin, appear to play critical roles in the sex disparity of liver cancers.
Using a liver tumour model in krasv12 transgenic zebrafish, a research group led by Prof GONG Zhiyuan, including Ph.D. students YAN Chuan and YANG Qiqi from the Department of Biological Sciences, NUS found that some other factors which are not sex hormones play critical roles in the sex disparity of liver cancers. In one study, they found that a glucocorticoid hormone, cortisol, is produced more than usual in male zebrafish with liver cancers. This hormone could trigger two different types of white blood cells, neutrophils and macrophages, which in turn enhance the development of liver cancer. In another study, they found that serotonin, a neurotransmitter, is also produced more than usual in male oncogenic livers. This again can cause the growth of liver cancer through the activation of a major cell type involved in liver diseases (hepatic stellate cells).
Zebrafish liver tumours share remarkable similarity with human liver tumours in terms of disease markers, molecular pathways and other features. The current studies provide the first evidence showing the involvement of non-sex hormones in male-biased liver cancer. These findings have also been validated in human liver disease samples. Apart from strengthening confidence in using zebrafish to study human liver cancers, it can lead to new potential therapeutic targets for the treatment of liver cancers. This can also be extended to other types of cancer which show sex disparity, particularly those found in the digestive tract.
Although two major molecular pathways have been identified in enhancing male-biased liver cancer, the detailed molecular mechanisms involved remain unclear. In particular, the mechanism in which the activation of the kras oncogene can trigger the two molecular pathways remains unknown. The present studies have focused on the roles of neutrophils, macrophages and hepatic stellate cells. However, the contribution of many other types of liver cells within the tumour microenvironment, such as bile duct cells, other immune cells and platelets, etc. remains to be studied. There is a need for a more comprehensive understanding of the tumour microenvironment so that a more effective cure against liver diseases can be developed.
Prof Gong commented, “The zebrafish model is increasingly used for human disease studies and now all major universities and research institutes around the world have established zebrafish facilities for biomedical research. The current studies highlight the importance of some non-sex hormones in the development of male-biased liver cancer and this may prompt us to have alternative and supplementary therapeutic strategies in fighting it.”
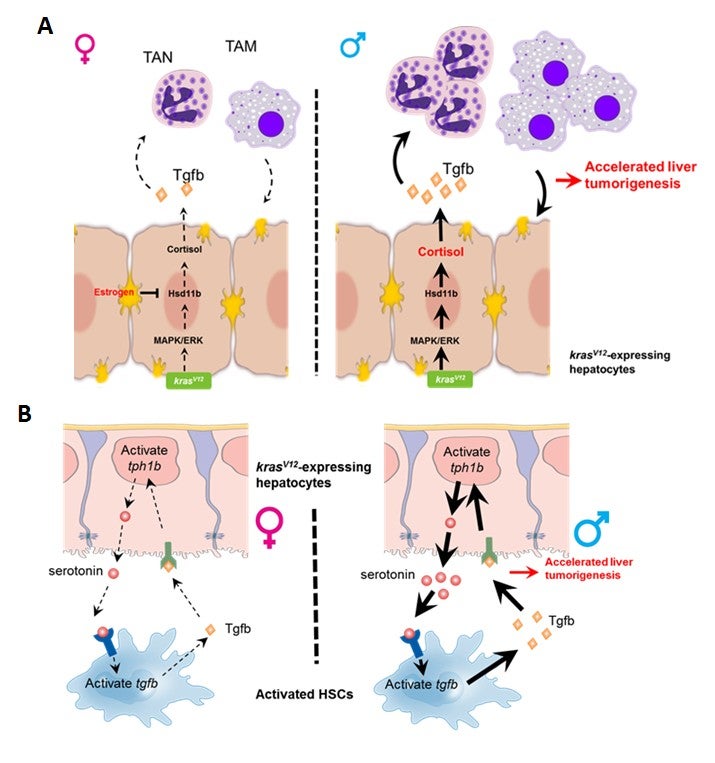
Figure shows the schematic illustration of (A) cortisol and (B) serotonin pathways in male-biased development of liver cancer. Abbreviations: TAM: Tumour-infiltrated macrophage; TAN: Tumour-infiltrated neutrophil; HSCs: Hepatic stellate cells.
References
Yan C; Yang Q; Gong Z*, “Tumor-associated neutrophils and macrophages promote gender disparity in hepatocellular carcinoma in zebrafish” CANCER RESEARCH Volume: 77 Issue: 6 Pages: 1395-1407 DOI: 10.1158/0008-5472.CAN-16-2200 Published: 2017.
Yang Q; Yan C; Yin C; Gong Z*, “Serotonin activated hepatic stellate cells contribute to sex disparity in hepatocellular carcinoma” CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY 3(3):484-499 DOI: 10.1016/j.jcmgh.2017.01.002 Published: 2017.


